An Introduction to the immune system
At any given point in time, the invaders of our body include viruses, bacteria, fungi, worms, and many other organisms. The immune system prevents pathogens from getting too comfortable inside us and mounts a response to destroy them if they enter the body. It, therefore, has the excellent ability to distinguish self from non-self.
Innate immunity, the primary line of defense, is a non-specific arm of the immune system that reacts to any foreign substance or organism. Our skin, the largest organ of the body, acts as a mechanical barrier to the outer world. The secretions of the mucous membranes lining our respiratory, stomach, gut, urinary, and genital tracts trap microbes to prevent them from entering deeper into our body. The many arms of our innate immunity include the acidic pH inside our stomachs, the rise in the body temperature characteristic of a fever, and the presence of lysozyme in our tears and saliva that breaks the cell walls of bacteria. Phagocytes like dendritic cells and macrophages are also deployed to engulf and ingest these invaders and destroy them to prevent any further mayhem.
When someone gets a mosquito bite, a cut on their skin, or even a heart attack, inflammatory responses are observed, usually as redness, swelling, heat, and pain. Mast cells are one category of the immune cells that are constantly patrolling the body and when they encounter any foreign body, they release histamines to signal for blood flow to increase to that area and stimulate inflammation. Further, neutrophils and macrophages come to the infected area to destroy the infected cells and the pathogens. There are many other components of the innate immune system –The complement system, Toll-Like Receptors (TLRs), and dendritic cells — many of which can also feed into the adaptive immune system.
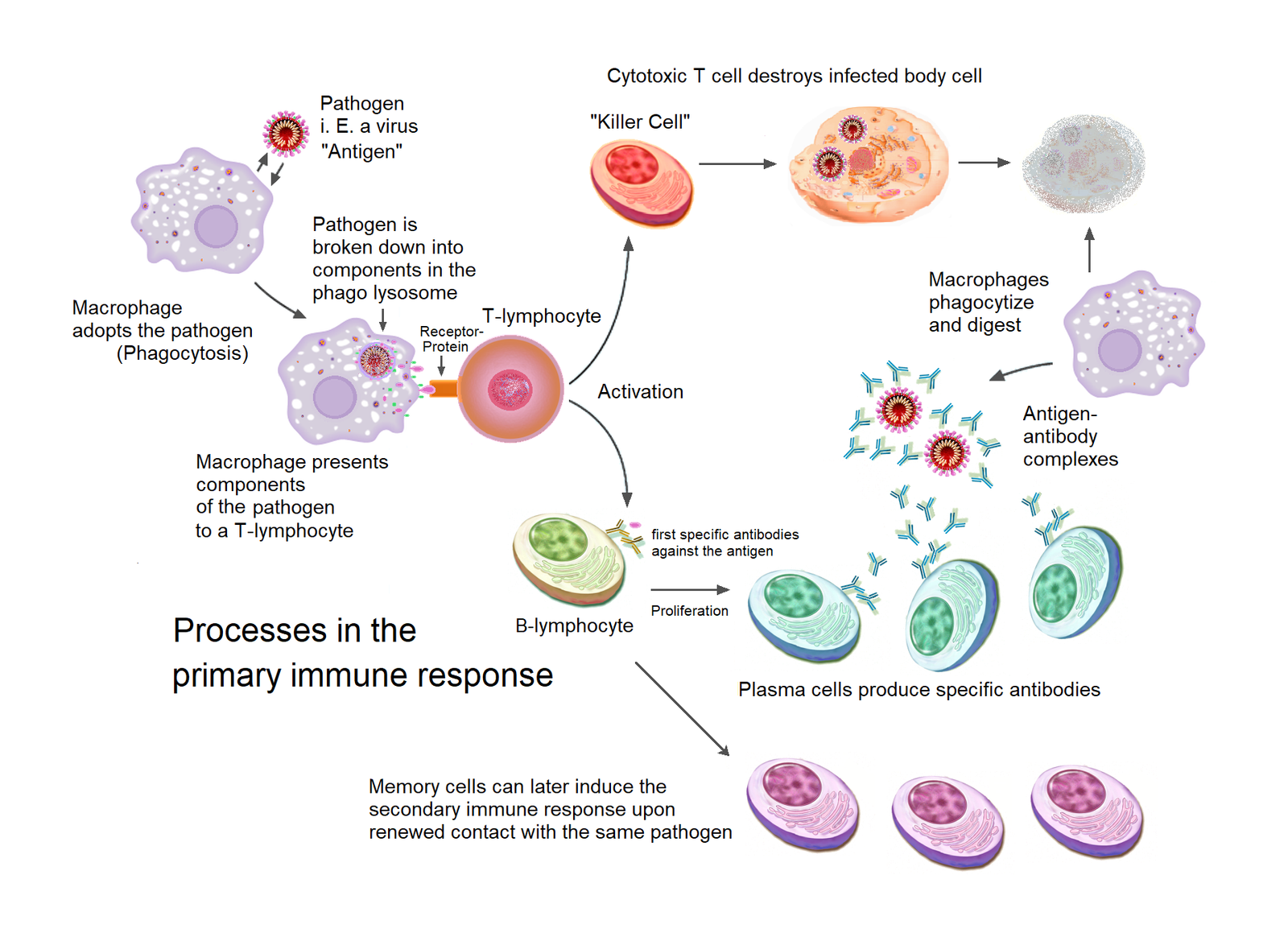
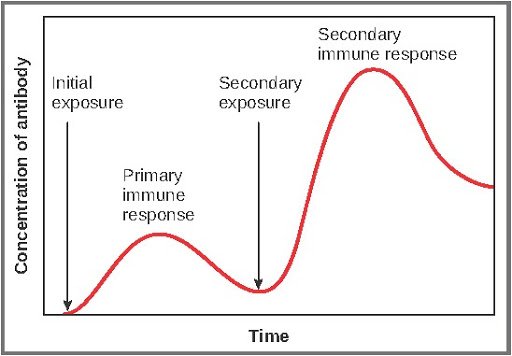
The adaptive immune system, on the other hand, is a much more specialized defense response that kicks in after the initial innate response. The adaptive immune response is armed with two kinds of cells, B cells, and T cells, that counter the pathogens that have invaded the body (and in some cases, even survived the initial immune attack). T cells, with their myriad subtypes, perform multiple specific functions – They summon other immune cells to help launch the attack, carry traces of pathogens already killed for current and future reference, and even kill the infected host cells that can no longer recover. Meanwhile, B cells churn out millions of antibodies that identify specific antigens, which can be proteins, lipids, or other biomolecules unique to the infectious organism for phagocytes to recognize them. Further, memory B cells along with T cells keep the record of all the previous infections, sometimes for the rest of your life. This is why, for example, people who have had chickenpox once are unlikely to get it again. This happens because the strong memory of the past encounter helps the immune system deactivate the chickenpox virus upon its re-entry before it can cause much damage to the body. But it is important to keep in mind that the immune system’s memory may not be life long for every single infection and depends on selecting the cells that produce the right antibodies, the type of pathogen and how it evolves.
Resources
- [UG] Innate immune defenses – details on how the body recognizes foreign particles or organisms as “Pattern recognition receptors”, makes use of cytokines, and other leukocytes(phagocytes).
- [UG] Adaptive immune defenses and Antibodies – details on antibodies, cell-mediated and humoral immunity, memory of the immune system; antibody types and their order of secretion to fight the infections.
- [UG] The complement system – briefly describes the functions of the complement system.
- [UG] The inflammatory response – details on the cytokine- Tumor necrosis factor-alpha (TNF-alpha) and the results of it along with the typical signs of inflammation.
- [UG] The following tables summarize the different cells of the innate system alongside the descriptions. The neutrophils, monocytes, macrophages, basophils and eosinophils are categorized under white blood cells. All of these originate from a myeloid progenitor cell along with mast cells and dendritic cells. But some dendritic cells can originate from lymphoid progenitor cells.
- [Classes 6-8] Infectious disease case study – (Students use evidence to determine whether a patient has acold, flu or strep infection, and they also learn the differences between bacterial and viral infections. This activity is from The Science of Microbes Teacher’s Guide, and lessons from the guide may be used with other grade levels as deemed appropriate.)
Face-off with the virus
Once viruses hijack the cellular machinery, cells have the ability to display parts of viral proteins on their surface using tag-like protein molecules, called Major Histocompatibility Complex(MHCs). This presentation is noticed by a particular class of T cells known as cytotoxic T cells, which then release molecules that puncture holes into the infected cells and start a cascade of reactions to cause cell death. Other times, when these MHCs do not carry cellular proteins or any viral proteins, they are detected by Natural Killer cells and meet the same eventual fate – the infected cells are killed, preventing the spread of infection to other cells. The cells taken over by the viruses also release interferons, a type of cytokine that prevents viral replication within the cell while also warning the neighbouring cells of the attack. Soon after, B cells produce antibodies that bind specifically to proteins on the surface of the virus. The neutralized virus, having multiple antibodies bound to it, can no longer use its surface proteins to bind to our cells and infect them. Finally, the neutralized viruses are recognized and destroyed by specialized macrophages of the particular organ in which the infection has occurred.
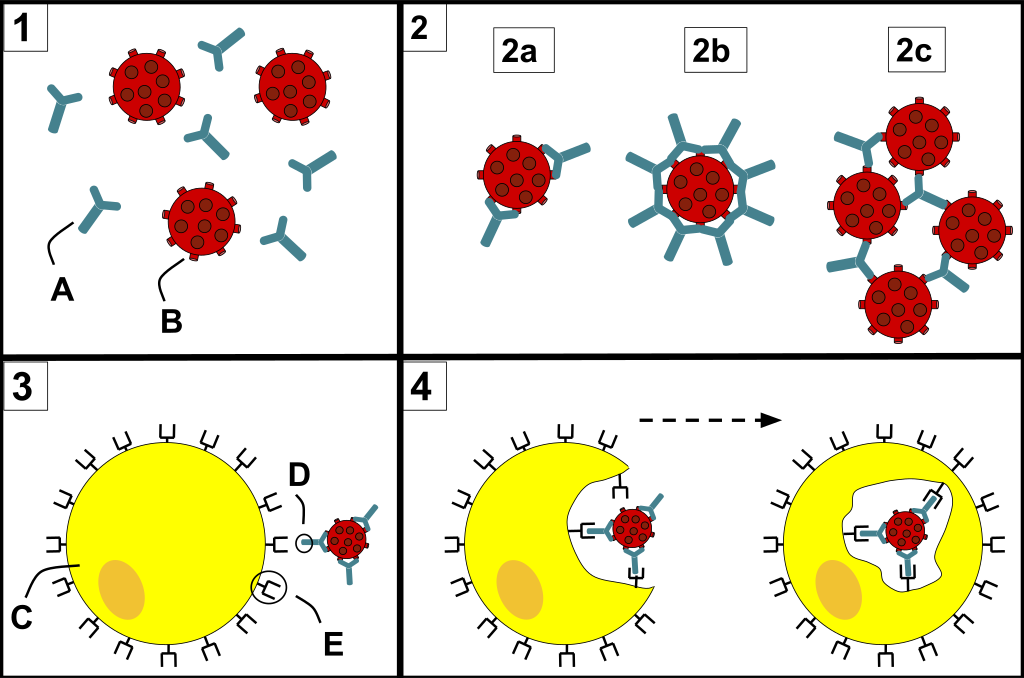
3) C represents a phagocyte approaching the pathogen attached to the Fc region(D) of the antibody. These Fc regions of the antibodies bind to the Fc receptors (E) on the phagocyte.
4) Phagocytosis occurs as the pathogen is ingested.
(Image: Wikimedia)
Resources
- [HS and UG] Immune responses to viruses – The basics of how the immune system targets viruses – explained by detailing the actions of cytotoxic cells (T cells and Natural Killer cells), interferons, and antibodies.
- [HS] Virus Wars – A Star-Wars themed page explaining how our immune system uses antibodies to fight viruses. It answers: what is a virus?, fascinating facts about viruses, antibodies strike back, antibodies, antigens and antibiotics, are viruses alive? and defines vaccination.
- [HS and UG] How The Body Reacts To Viruses – HMX – This page consists of multiple sections, each explaining a type of immune response (B cell response, T cell response, etc) along with a set of great graphics/slides for each. The last section focuses on the immune response to viruses in particular.
- [UG] Interfering with Interferon – This short post starts with explaining how cytoplasmic proteins recognize viral RNA as foreign and induce IFN production. Though, it’s from the perspective of a few experiments run from two groups and is written in the form of an open narrative.
The interaction of the human body with SARS-CoV-2
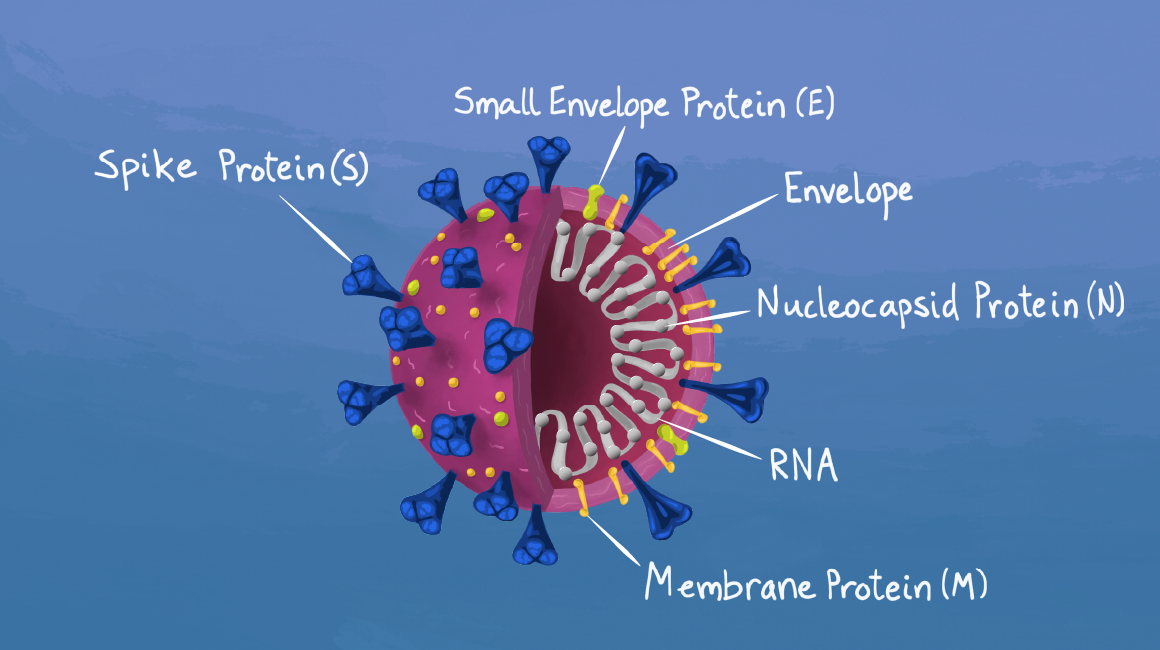
Coronaviruses are a family of viruses that contain genetic material made of RNA, which is enveloped by a lipid membrane embedded with proteins.
Out of the seven coronaviruses known to infect humans so far, four cause a common cold. The other three, SARS CoV (Severe Acute Respiratory Syndrome Coronavirus), MERS CoV (Middle East Respiratory Syndrome Coronavirus), and SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus-2), cause much more severe forms of respiratory illness.
SARS-CoV-2, the most recently discovered coronavirus, causes a disease called COVID-19, which has infected millions as it continues to sweep across the world. The disease can be mild in some cases, and in other cases cause devastating damage and even death.
SARS-CoV-2 spreads mostly through droplets that are released during coughing, sneezing, singing or even talking while facing the other person. The virus particles in these droplets usually enter our body through our nose. Early reports show that depending on the number of virus particles that gets transmitted, there might be different scenarios – the infection can start in the throat, and may get cleared off by the innate immune response, thus preventing the virus from reaching the lungs. In other cases, if a large number of viruses enter the body, they can directly infect the lungs.
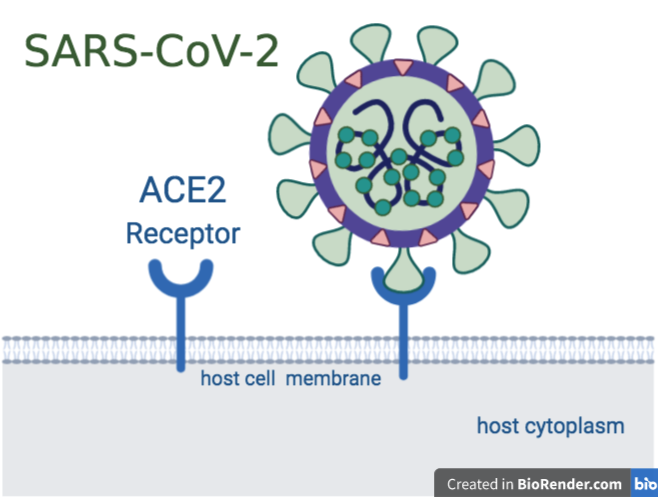
Coronaviruses have special surface proteins called spike (S) proteins. SARS-CoV-2 uses these to bind to the receptor ACE2, which is present on the surface of our lung cells. The spike protein is cleaved by host cell processes to enable entry into host cells. Once inside, the virus uses the cellular machinery to replicate the viral genetic material and thus make more copies of itself. Once enough copies of the virus are made, the newly-formed viruses burst out of the cell, causing the cell to die. A healthy immune response to this viral invader would mean a controlled cascade of inflammatory molecules, followed by T cells and virus-specific antibodies from B cells, as explained above. And in many cases of COVID-19, this is indeed how the virus is fought off. In such instances, the patient only develops a very mild infection, or in certain cases, no apparent infection at all.
Resources
- [HS and UG] There are more viruses than stars in the universe. Why do only some infect us? – In the context of the SARS-CoV-2, this article talks about everything that needs to go right for viruses to find the perfect host – zoonosis (in many cases), the perfect and flexible genetic code of the virus, the perfect host cell receptor the virus can fit into – and everything that can make the virus the “perfect pathogen”.
- [UG] Profile of a killer: The complex biology powering the coronavirus pandemic – A Nature article on the first known cases of coronaviruses, their family of viruses, the origin of SARS-CoV-2, the way they cause infections inside the human body with a comparison to SARS-CoV and MERS and how it might end?
- [UG+] Infographic – A defective vs healthy immune response to the SARS-CoV-2 – An infographic from a Nature Reviews Immunology article, highlighting the differences between a healthy immune response (action of neutralizing antibodies, minimal inflammation, etc) and an unhealthy immune response (widespread inflammation, rampant cell death) against SARS-CoV-2 during COVID-19 infection.
- [UG] Why immunity to COVID-19 is so complicated – A basic overview of how the immune system works, also highlights the inconsistencies of antibodies and talks about how re-infection can elicit different responses in different individuals.
Cytokine storms: a defective immune response
However, in severe cases of COVID-19, symptoms manifest as pneumonia, ARDS (Acute Respiratory Distress Syndrome), and even multiple organ failure, leading to death. While research is still uncovering how the virus affects different parts of the body, causing widespread damage, it is already well known that these symptoms are also a manifestation of our immune system going into overdrive.
Cytokines are an essential part of a healthy immune response. However, when these molecules are produced in excess, they lead to a cytokine storm, causing widespread inflammation and a vastly exaggerated immune response. This causes an overload of immune cells and debris to fill the lungs (usually the site of infection), thus disrupting oxygen transfer. This is how the patient develops pneumonia. As oxygen levels in the blood plummet further, this could lead to Acute Respiratory Distress Syndrome (ARDS), at which point the patient has to be put on oxygen support.
Cytokine storms also cause widespread thrombosis (blood clotting). Blood clots of different sizes then travel to different parts of the body (heart, brain, lungs, kidneys, etc) and cause havoc by impairing oxygen supply to the organs. Furthermore, the extreme levels of inflammation can injure the heart muscle, thus leading to heart attacks among many COVID-19 patients, even those who have had no previous history of heart disease. This is also worsened by the lack of oxygen-rich blood supply to the heart since the lungs themselves are affected.
Resources
- [HS and UG]What is a cytokine storm?– Explains the basics of cytokine storm, why COVID-19 patients have an avalanche of cytokines and if that can lead to death?, compared to the cytokine storm in H1N1 Flu, medicines used to treat such hyper inflammatory responses in different diseases yet.
- [HS and UG] How does coronavirus kill? Clinicians trace a ferocious rampage through the body, from the brain to toes – This Science Magazine article is from the perspective of health-care physicians who discuss how SARS-CoV-2 takes over different parts of the body apart from the lungs only. The subheadings are – Infection begins, An invader’s impact, Striking the heart, Multiple Battlefields, Buffeting the brain, Reaching the gut.
- [UG] Spider man immune response may promote severe COVID-19 – This article talks about research that links a severe COVID-19 response to a high count of Neutrophils in the patient’s body. The “Spider-Man” Maneuver, wherein neutrophils shoot sticky webs of DNA and toxic proteins (called Neutrophil Extracellular Traps) to trap the pathogen, though useful, causes the involved neutrophils to die and may do more harm than good in a patient infected with COVID-19.
- [UG] The Perfect Storm – This short article briefly describes co-morbidities in severe COVID-19 infections and then elaborates on the concept of a cytokine storm – why it arises (increased viral load, death of T-cells), and its effects throughout the body (blood clot formation leading to secondary effects and even organ failure).
Differences in susceptibility to pathogens
Different people respond to COVID-19 infection in different ways – some are more susceptible, some have an exaggerated immune response, others are asymptomatic. One of the reasons is that there are genetic differences contributing to slightly different versions of the MHC protein (due to variations in the MHC antigen loci), that affects people’s susceptibilities to disease. Susceptibility also depends on age – the elderly are far more susceptible than children and normal adults. People with co-morbidities such as diabetes, TB, and hypertension are also at a greater risk of severe COVID-19 infection. Another group of people at high risk are those who are on medication after organ transplants, and those whose immune systems are greatly weakened by diseases such as cancer and AIDS. Such people are immunocompromised, and unable to launch a strong enough attack against invading pathogens.
Resources
- [UG] Immunity and immunopathology to viruses: what decides the outcome? – This Nature Reviews Immunology review article focuses on the host factors that play a role in viral infection – genetic predisposition, inflammation responses, age of host during infection, etc.
How vaccines work
A vaccine usually consists of a dead or weakened form of the pathogen and is administered to the body to allow our immune system to respond. Sometimes, specific antigens or even genetic material (which by themselves cannot cause infection) from the pathogen are used to trigger our immune system to develop antibodies against them.
Most of the developments surrounding SARS-CoV-2 vaccine candidates have come from using its spike protein. Moderna’s mRNA vaccine, mRNA 1273, delivers the genetic code (in the form of RNA) of the spike protein to the cells. Once inside the cells, the RNA is converted to the functional spike protein, which then acts as an antigen to elicit an immune response. The University of Oxford and the company AstraZeneca are making use of a chimpanzee adenovirus to carry the SARS-CoV-2 Spike DNA, which, upon reaching the cell, can be converted into its protein antigenic form. On the other hand, Sinovac Biotech from China is testing a vaccine candidate (Coronavac) that uses the entire inactivated virus, and not just specific antigens. Even though vaccines take years to become available to people as adequate time is required for development, testing, and safety checks, these efforts have already reached phase 2 trials. However, these vaccines still need to undergo vigorous testing and clinical trials before they can be deemed safe enough to be administered to the public.
Resources
- [UG]Genetic Engineering Could Make a COVID-19 Vaccine in Months Rather Than Years – A Scientific American article on types of vaccines, development of a viral vaccine against SARS-CoV-2 and its phases of clinical trials. It is accompanied by a graphical guide which is a major highlight in this article.
- [UG] The race for coronavirus vaccines: A graphical guide – A Nature article on basics of vaccine-How we develop immunity? And types of vaccines against viruses- Viral vector vaccines, Nucleic acid vaccines and Protein-based vaccines.
- [UG] COVID-19 Vaccine developers search for antibodies that first do no harm – This article focuses on the efforts of vaccine development against the SARS-CoV-2. It discusses the potential dangers of vaccines (developed in haste in the current scenario) to cause Antibody-mediated Enhancement where the immune system can trigger a harmful inflammatory response instead of keeping the memory for the real infection.
- A COVID 19 vaccine has passed its first human trial. But is it the forerunner? – This article details how mRNA vaccines are developed and why they weren’t in use for a long time. Also, it tells the story in relation to Moderna’s mRNA vaccine trials.
- [Grade 4-8] Classroom resources for teachers (a) Vaccine-preventable diseases-A CDC resource – Body and Mind –Diseases and vaccines that prevent them-(Chickenpox, Diptheria, flu, Hepatitis A, Hepatitis B, HPV, Measles, Mumps, Polio, rotavirus, rubella, etc) (b) Vaccine basics -Definition-immunity, vaccine, vaccination, immunization; Why immunize? How does immunity work? etc)
- [UG] Mullard A. World Report COVID-19 vaccine development pipeline gears up. Lancet. 395(10239):1751-1752. doi:10.1016/S0140-6736(20)31252-6 – This paper highlights the current vaccines in the trial(updated till June first week), the potential shortcomings of the vaccines in development and what it means for herd immunity.
Plasma Therapy in treating infections
Convalescent Plasma Therapy is a form of treatment wherein plasma from a recovered individual who had the disease is transfused into a current patient since the plasma would contain antibodies specific to the pathogen.
A person who is infected with COVID-19 for the first time has no prior SARS-CoV-2 specific antibodies in their blood. By the time their body actually produces these antibodies, it is possible that the virus could cause too much damage, or the immune system could go into overdrive. Therefore, making it possible to “borrow immunity” in the form of ready-made antibodies from a willing donor can help halt the virus in its tracks and potentially save the patient’s life.
Resources
- [HS] What is convalescent plasma? – This article explains the meaning of convalescent plasma, the use in previous infections, method of extracting plasma from a recovered patient, and who receives the treatment.
- [UG+] Convalescent plasma in Covid-19: Possible mechanisms of action – This review article elucidates the possible mechanisms of action of Convalescent plasma therapy (neutralization of virus, suppression of an overreactive immune response, etc) with particular reference to COVID-19.
Herd Immunity
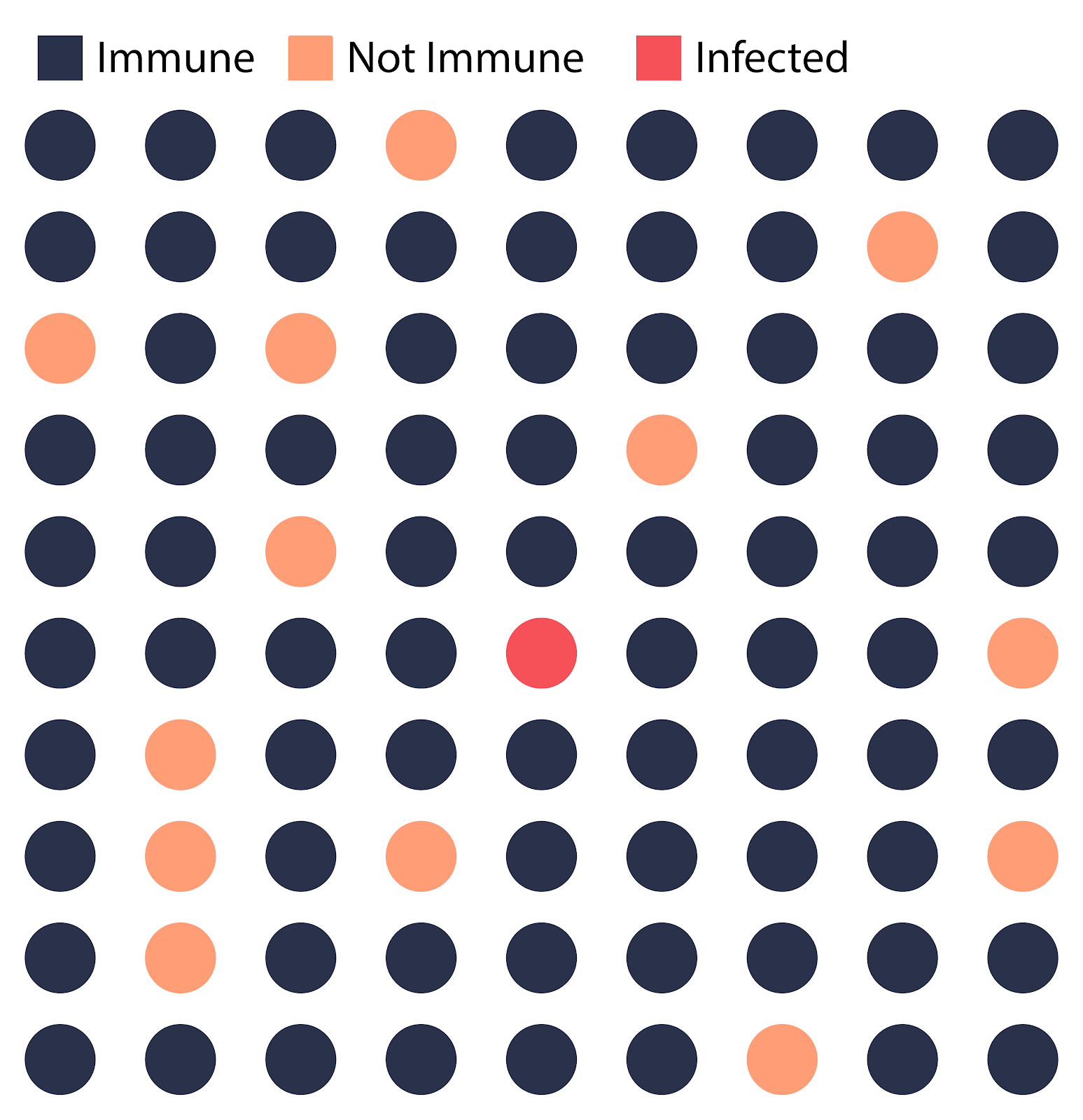
The spread of a disease across a community can stop only if a large proportion of the people in that community are immune to the disease. Herd immunity is a term used to describe the indirect protection that susceptible people have against a disease, due to the fact that most of the population is immune to the disease.
How can herd immunity be achieved? The first way is quite straightforward – if enough people are infected, they will eventually gain immunity to the disease and prevent a second outbreak. Understandably, this cannot work for life-threatening diseases such as Ebola or even COVID-19, as too many lives are at risk. However, if a majority of the population is vaccinated (the exact percentage varies across diseases), these people will no longer be a part of the transmission chain of a disease, thus preventing a potential outbreak. This is why large-scale vaccination programs are so important. Essentially, herd immunity protects the fraction of the population that cannot receive vaccines – immunocompromised individuals, and certain people whose immune systems do not respond to vaccination.
There are still many questions to be answered about potential drugs and vaccines, and as to why the immune system responds unpredictably in different situations and different individuals. As a complex, multi-faceted collection of cascades and processes, more is uncovered about our immunity with each new disease that strikes us.
Resources
- [UG+] What immunity to COVID-19 really means – Scientists are still trying to find out whether SARS-CoV-2 can provide immunity to the recovered people after the infection. This article focuses on giving some competing ideas in the field about the level of immunity of SARS-CoV-2 and measuring the neutralizing antibodies(if sustained for a long time in people infected) to know the spread of the pandemic.
- [HS] What is herd immunity and how can we achieve it for COVID-19? – This article explains the use of vaccines in case of decreasing the spread of other infectious diseases and later elaborates in the context of SARS-CoV-2.
- [UG] What the proponents of ‘Natural’ herd immunity don’t say – This NY Times article discusses the potential use of vaccines to propagate immunity in a population and warns the idea of naturally developing natural immunity. Also, it points to the controversy of yet known state of the immunity conferred by a coronavirus.
Video Resources
- [HS] The Amoeba Sisters:Immune System 8:55- This video details the immune system- first line of defense(skin and mucous linings), second line of defense(white blood cells and phagocytes) and third line of defense(B cells and T cells).
- [HS] Ted-Ed: How does our immune system work? 5:22- This video focuses on showing how the immune system is an intricate connection between cells, tissues and organs of the body. It briefly elaborates on leukocytes, their types (phagocytes and lymphocytes) and functions.
- [HS] Science ABC: Immune system: Innate and adaptive immunity explained 7:10 – This video describes the two branches of the immune system. It starts with the primary defense (skin, mucous lining, tears, acid in stomach, microbiome flora in the body), explains the process of inflammation, antibody production, and memory retention.
- [HS] Kurzgesagt – In a Nutshell: The Immune System Explained I-Bacterial Infection 6:48 – This video is different in approach as compared to the other videos as it focuses on the scale of the immune cells, the function they do and provides the contextual reference to bacterial infection.
- [HS] Kurzgesagt – In a Nutshell: Tiny Bombs in your blood- The Complement System 8:40 – An excellent video on the need of a complement system to the immune system of the body and what the specific functions of the complement system are?
- [HS and UG] What Actually Happens If You Get Coronavirus? – This video discusses viruses in general, then moves to describe the SARS-CoV-2 and the way it infects the body and the immune response.
- [HS] 5 Minute School: How does the body fight a virus? 3:16 – This video elaborates on the MHC found in normal cells, the changes a cell undergoes on infection to attract cytotoxic T-cells or Natural Killer Cells, neutralization of viruses by antibodies.
- [HS] Oxford VaccineGroup: How does herd immunity work? 2:46 – This video explains how the use of vaccines prevents the spread of diseases, and where it doesn’t work.